It’s often little gestures that can have the biggest impact.
It may be helping a senior with technology so they can have a virtual call with family, helping a patient with dementia at mealtime, or resolving an issue from the complex to the simple.
In all those cases, the act of listening and journeying with a patient or resident is the particular skill of the four-member Patient Relations team at Covenant Health. Their mandate is to help make the experience of being in a hospital or health facility as positive as it can be — even in the midst of the COVID-19 pandemic.
“Despite the difficulties, every day we see individual staff members do those incredibly thoughtful, actions of human-connection that make a real difference for our patients and families. We get to hear difficulties but we also get to hear when things work well,” said patient relations manager Joy Hurst.
“Teams throughout Covenant Health have really facilitated virtual contact,” Hurst said. “That’s new for some people, particularly generationally. For young people that’s just life, but for many older people this is new.
Early in the pandemic, “It was wrapping somebody up in a blanket and taking them to a window where they could wave, and making sure the family on the other side was located in a good spot so they could communicate with each other. Just taking that time.”
World Day of Prayer for the Sick, established by St. John Paul II about a year after he was diagnosed with Parkinson’s disease, is celebrated on Feb. 11 this year. Locally, Archbishop Richard Smith has recorded a video message of encouragement, gratitude and prayer for those who are sick or tend the sick.
In his own message, Pope Francis emphasized the value of relationships in care and recovery:
“Emphasizing this aspect can help doctors, nurses, professionals and volunteers to feel responsible for accompanying patients on a path of healing grounded in a trusting interpersonal relationship,” the Holy Father wrote.
“This creates a covenant between those in need of care and those who provide that care, a covenant based on mutual trust and respect, openness and availability. This will help to overcome defensive attitudes, respect the dignity of the sick, safeguard the professionalism of healthcare workers and foster a good relationship with the families of patients.”
Hurst, and her Patient Relations team at Covenant Health, deals with this every day.
“Sometimes what we’re doing is journeying with somebody, just walking beside them. That makes a huge difference in giving them confidence and hope,” she said.
The Patient Relations team is on-call to field compliments, concerns, and sometimes suggestions, from those receiving care at all 18 Covenant Health sites in Alberta. Public feedback can range from parking lot issues, food quality, bed availability, or identifying and resolving an issue with a patient, resident or family member. That’s especially true amid COVID-19, when health staff have to be creative in improving the experience in a health facility while under pandemic restrictions.
“We never expected something like this,” Hurst said. “You can’t do this work and hear the stress of patients, families and staff without being affected by the burden of distress that is being experienced during this pandemic. This is one time where that tension between the community good and the individual good, is literally amplified every single day,” Hurst said.
Covenant Health has had a Patient Relations department since 2006, when it was still the Capital Health Region in Edmonton. Hurst said a survey prior to that inception, showed “the public had a hit-and-miss experience when they tried to bring things forward”. While all caregivers are responsible for a positive patient experience, Hurst’s time is a designated, intentional group to provide a structured response to public concerns.
“It’s important to have this be the sole priority of someone,” Hurst said. “This is our priority, to listen to patients, and to convey what patients have to tell us. That’s a good step in healthcare that’s very progressive.”
“We’re an advocate for good care. At the end of the day the purpose is to improve that individual experience, if there’s some problem-solving that can be done, or help navigate the system. Patient experience and perspective provides leaders with good information about how services are actually received…not how they think they were received, but the actual experience of patients, residents and families.”
And it’s not just a soft skill. The Patient Relations department sees a measurable difference.
“When there’s a positive relationship, patients are more likely to follow the advice given,” said Hurst, who’s been on staff since the department’s early days.
“They are more likely to take their medications and feel confident and comfortable in the recommendations. They are more likely to tell the practitioner personal things, things that the practitioner actually needs to know so they can make an informed decision on care and treatment. If you don’t have a good communication with someone, you’re not likely to tell them anything that you don’t have to.”
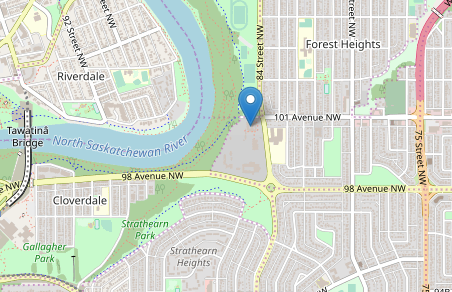
The Patient Relations team works from a building near the Misericordia Hospital in Edmonton. Almost all of their work is done remotely, even before COVID, because they serve all Covenant Health facilities. It initially took a bit of adjustment for Hurst, who has a background in social work and was accustomed to working with people in person.
“When people are distressed, sometimes they don’t mind when they’re talking to people on the phone,” Hurst said. “They have somebody who is listening to them. They have somebody who is taking action.”
What makes their work difficult, Hurst said, is when there’s an issue with the health-care system that can’t be resolved, or when her staff receive feedback after a patient or resident has died.
“I find that the hardest, because there’s very little that can be done after the fact,” Hurst said. “It’s very challenging when family haven’t come forward during that whole period they were receiving care. Hurst acknowledges that she and her staff deal with stressful situations, and it can affect them personally.
“You always are reflecting on things that have happened, but as long as the organization is learning, responding and adapting, that’s positive. That’s what we’re here to facilitate.”
And then there are the reminders of the need for, and impact of, their work. Hurst recalls a mother who recently received a call about a disturbing test result. “That’s really scary. That’s so scary when you hear ‘Something was abnormal and you need to come in.’”
Hurst’s first response was there was nothing her department could do. The health system process would unfold as it should in terms of timing. However, “as we often do, we take it one step further.”
She made some calls, got some advice, and with consent spoke with the patient’s family doctor and provided information regarding access to urgent specialty services. “At the end of the day, this patient — she has cancer — and the family continues to call me, grateful because we took that little bit of extra time to support them in navigating the system,” Hurst said.
“That made a real difference for her. She had confidence that somebody cared, somebody is interested. And that was impactful to them and impactful to me, because their feedback says that this work really does matter and does make a difference in how people experience their health care.”
What keeps Hurst and her department grounded is a quote from the Catholic Health Alliance of Canada’s Health Ethics Guide. Hurst isn’t Catholic, but the values articulated in that one paragraph mirror her own. It’s displayed prominently on her desk and on a poster in the office:
“Our distinctive vocation in Christian health care is not so much to heal better or more efficiently than anyone else; it is to bring comfort to people by giving them an experience that will strengthen their confidence in life,” the quote reads. “The ultimate goal of our care is to give those who are ill, through our care, a reason to hope.”