At what point does a health care provider become complicit in the act of medically assisted death?
As more patients seek euthanasia or assisted suicide in Alberta, Covenant Health – one of the country’s largest Catholic health care providers – is gaining more experience in making that call.
“We’re not going to participate in ending someone’s life prematurely,” said CEO Patrick Dumelie. “It really stems from the belief that we respect life from conception to natural death.”
As of Sept. 30, there have been 486 such deaths in Alberta since “Medical Assistance in Dying” (MAID) was legalized in June 2016. Of those, 64 patients were transferred from a faith-based facility that does not provide the service.
Covenant Health was not able to provide the number of its patients who have requested medical assistance in dying or the number who have been transferred from its sites for assessments.
But at least one of those transfers didn’t go smoothly.
In the spring of 2017, Doreen Nowicki was 66 and terminally ill with amyotrophic lateral sclerosis, also known as ALS or Lou Gehrig’s disease.
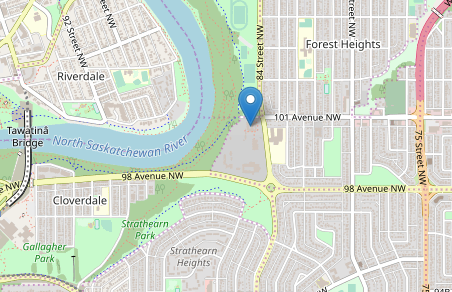
She was receiving palliative care at the Edmonton General Continuing Care Centre operated by Covenant Health. CBC News reported on Oct. 23 that she was forced to have her assessment for medically assisted death on the sidewalk outside the facility.
Covenant Health issued an apology.
“We didn’t do everything we should’ve done to support this patient and family,” Dumelie said.
“It’s really important for us as a compassionate, caring organization living our mission, that we don’t abandon people when they’re at their highest need. And so if you’re contemplating taking your own life, there’s no time that you’re more vulnerable. Something like this is really an adverse event. This isn’t how the system functions.”
Nowicki’s request to die was eventually met through Alberta Health Services. For its part, Covenant Health has apologized to the family and learned from the experience, Dumelie said.
Covenant Health considers healthcare an “immense responsibility and a calling,” Ed Stelmach, the board chair and former Alberta premier, said at its annual community meeting on Oct. 24.
“It’s also challenging work and sometimes we don’t get it right, as you might have read in the news,” said Stelmach. “It requires humility and a commitment to learn and improve.”
Dr. Owen Heisler, Covenant Health’s chief medical officer, said the Catholic health care provider has since improved its system of determining who may have medically assisted death assessments done on its premises and who should leave their facility for assessments.
Covenant Health participates in some of Alberta Health Services’ five stages that people go through when they are considering medical assistance in death, including the “Pre-Contemplation” stage, where a patient is seeking information, and the “Contemplation” stage, where they might make an informal or formal request for more information.
Covenant Health does not participate in the third stage, “Determination,” where assessments are done to see if they meet the criteria, or the fourth stage, “Action,” where the patient’s life is ended.
The fifth stage, “Care after Death,” is where grief support and follow-up is provided for the family.
“After that happens, there’s a lot of distress. We talk to the family to make sure the loved one is respected and the family is respected,” said Heisler.
The assessment stage, where an AHS navigator, or coordinator, meets with the patient and the family to determine whether the patient is a candidate for medical assistance in dying, is not allowed to be done on Covenant Health premises. Exceptions can be made in the case of “an extraordinary need,” said Heisler, such as a patient who is frail, or not physically able to leave the site.
“We look at it on a case-by-case basis, and we’ve actually found that quite a few people that come to us are in that category,” said Heisler.
The Covenant Health policy providing exceptions to having assessments done on site is a measure of compassion, Dumelie said.
“We don’t want to do more harm to the individual. We’ll journey with them, but we won’t participate in ending their life.”
When a patient is considering medical assistance in dying, Covenant Health’s policy is to seek ways of improving their palliative care, Dumelie added.
“Often people will seek out MAID because they don’t have the services and supports, they feel they are a burden on their family, their life has no purpose, the pain is too great. Today, with the kind of palliative care services we offer, we can address those issues for people and allow them to die with what we would say is true dignity.”
Covenant Health has garnered praise for its palliative care services from families such as the daughters of Margie Harper, a Castor woman who died at Our Lady of the Rosary Hospital in April 2017, after a full 30 days of end of life care in the hospital.
“I believe that our experience speaks to the philosophy of the Catholic hospitals’ real respect for life and real respect for the dying and for their families,” her daughter Carolynn Bilton said.